Test Your Basic Knowledge About Clotting Factors and Anticoagulants
Blood clotting and blood-thinning medicines are topics many people hear about but do not fully understand. You may come across these terms after surgery, during pregnancy, while caring for an older family member, or when reading lab reports. This guide is written in simple language and is meant to help students, patients, caregivers, and curious readers build clear basics.
You will learn what clotting factors are, how the body forms clots, why anticoagulants are used, and how common medicines work. Along the way, you will see practical tips, real-life examples, and small learning checks so you can test your understanding.
The goal is not to overload you with medical language, but to explain things in everyday words.
What Does Blood Clotting Mean in Daily Life?
Blood clotting (also called coagulation) is your body’s natural way of stopping bleeding. If you cut your finger while cooking, the bleeding slows down and stops after a short time. That is clotting in action.
Without clotting, even small injuries could become dangerous. With too much clotting, blood vessels can become blocked, which may cause serious problems like stroke or heart attack.
So the body must keep a careful balance.
Simple example
Imagine a small leak in a water pipe.
- Platelets act like quick patches that stick to the hole.
- Clotting factors act like glue that hardens and seals the patch.
- Once healing starts, the body slowly removes the glue.
This balance keeps blood flowing while still protecting you from bleeding.
Key points to remember
- Clotting protects you from blood loss.
- Too little clotting leads to bleeding.
- Too much clotting can block blood flow.
- The body uses clotting factors and platelets to manage this process.
Quick self-check
- Have you ever noticed how a scrape stops bleeding on its own?
- Did you know this process starts within seconds?
Coagulation Blood Clotting Factors
Coagulation, also called blood clotting, is the process that helps your body stop bleeding after an injury. This happens through a group of proteins known as clotting factors.
These factors are activated when a blood vessel is damaged. For clotting to work properly, you must have enough of all the clotting factors, and they must activate one another in the correct order.
Doctors often use blood tests such as PT/INR and APTT to measure how long it takes your blood to clot.
If you have unusual bleeding, unexpected blood clots, or abnormal PT/INR or APTT results, your doctor may request coagulation factor testing to understand what is happening.
These tests help show whether specific clotting factors are missing or not working as they should.
What is clotting factor testing?
Clotting factor tests measure the level and activity of individual clotting proteins in your blood. These tests help doctors investigate bleeding or clotting problems.
They are usually ordered in the following situations:
- After abnormal PT/INR or APTT results
- If you have a family history of clotting or bleeding disorders
- If you have liver disease or another condition that may affect clotting factor production
- To monitor clotting ability when you already have a bleeding or clotting disorder
- If you are taking medications that reduce clot risk
Some clotting problems are inherited, although this is uncommon. Others develop later in life because of illness or medication.
The Building Blocks: What Are Clotting Factors?
Clotting factors are special proteins in your blood. Most are made in the liver. They work together in a chain reaction to form a stable clot.
Doctors usually name them using Roman numerals, such as Factor I, Factor II, Factor VIII, and so on. Each factor has a specific job. If even one is missing or not working well, clotting can slow down.
Common clotting factors in simple terms
- Factor I (fibrinogen): becomes fibrin, the main “net” of the clot
- Factor II (prothrombin): helps start clot formation
- Factor V: speeds up the clotting process
- Factor VII: helps trigger clotting after injury
- Factor VIII: works closely with Factor IX
- Factor IX: important for stable clot building
- Factor X: central switch that leads to fibrin formation
- Factor XIII: strengthens the final clot
These factors do not work alone. They act in steps, one activating the next.
Why vitamin K matters
Several clotting factors depend on vitamin K to function. Without enough vitamin K, the liver cannot make working versions of these proteins.
Foods rich in vitamin K include:
- Spinach
- Kale
- Broccoli
- Brussels sprouts
This becomes important when people take certain blood thinners, which reduce vitamin K activity.
Practical tip
If you are on blood-thinning medicine, do not suddenly change how much leafy green vegetables you eat. Large swings can affect how your medicine works.
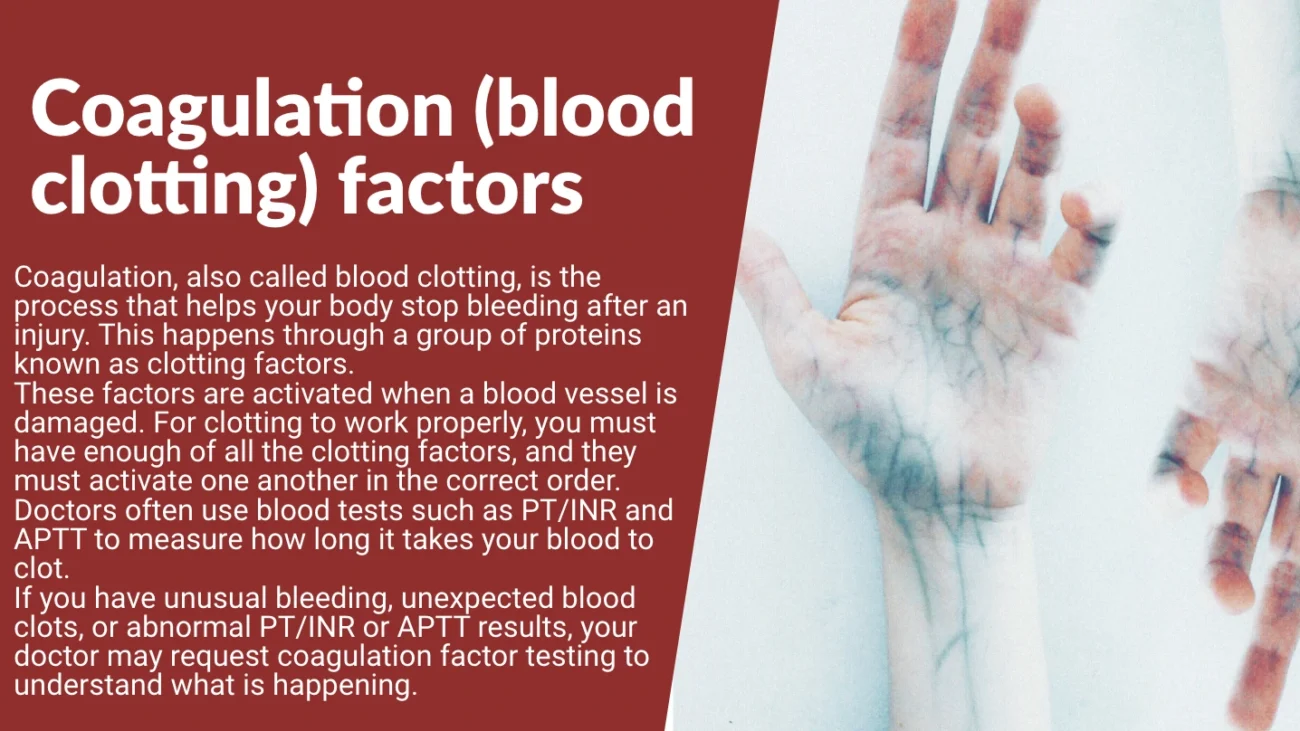
How the Body Forms a Clot: A Step-by-Step View
Clotting happens in stages. Each stage supports the next.
First stage: vessel injury and platelet plug
When a blood vessel is damaged:
- The vessel tightens to slow blood flow.
- Platelets rush to the site.
- Platelets stick together and form a soft plug.
This plug is fast but weak.
Second stage: clotting factor chain reaction
Next, clotting factors activate one another in a specific order. This produces fibrin threads.
- Fibrin wraps around the platelet plug.
- The plug becomes firm and stable.
Third stage: clot strengthening and repair
- Factor XIII tightens the fibrin mesh.
- Healing begins underneath the clot.
- Later, the body slowly breaks the clot down.
Summary in list form
- Injury occurs
- Platelets gather
- Clotting factors activate
- Fibrin forms
- Clot becomes strong
- Healing follows
When Clotting Goes Wrong
Problems happen when this system is off balance.
Too little clotting
This can cause:
- Easy bruising
- Long bleeding after cuts
- Nosebleeds
- Heavy menstrual bleeding
- Joint bleeding (in severe cases)
A well-known example is hemophilia, where certain clotting factors are missing or weak.
Too much clotting
This can lead to:
- Deep vein thrombosis (clots in the legs)
- Pulmonary embolism (clots traveling to the lungs)
- Stroke
- Heart attack
These events can be life-threatening and often need quick treatment.
Risk factors for abnormal clotting
- Long periods of immobility (long flights, bed rest)
- Smoking
- Certain cancers
- Pregnancy
- Some inherited conditions
- Older age
Anticoagulants: What Are They and Why Are They Used?
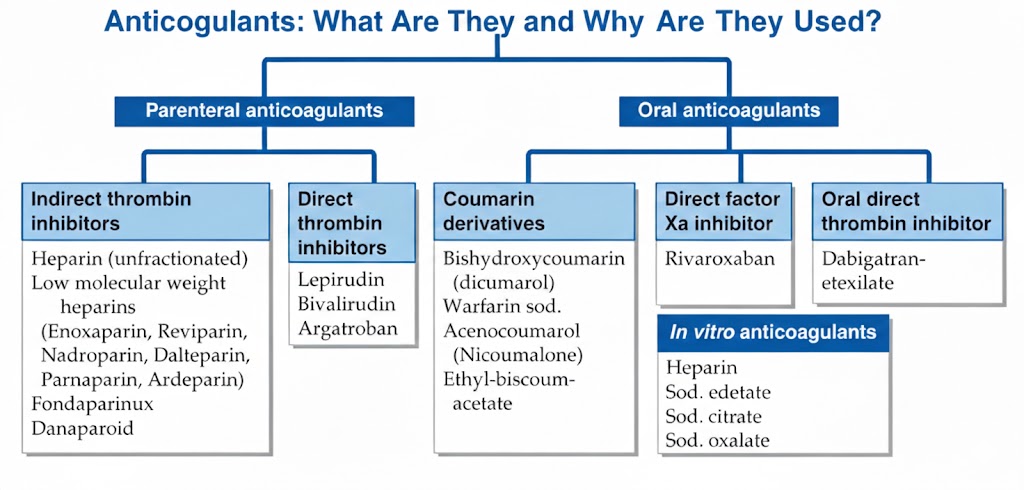
Anticoagulants are medicines that slow down clot formation. Many people call them “blood thinners,” although they do not actually thin the blood. They reduce the blood’s ability to clot.
Doctors prescribe anticoagulants to:
- Prevent strokes in people with irregular heartbeats
- Treat or prevent clots in the legs or lungs
- Protect artificial heart valves
- Reduce clot risk after surgery
Common goals of anticoagulant therapy
- Stop existing clots from growing
- Lower the chance of new clots
- Keep blood flowing smoothly
Everyday example
Think of traffic on a busy road.
- Clotting factors are like cars that can pile up.
- Anticoagulants act like traffic controllers, slowing things down so jams do not form.
Main Types of Anticoagulants Explained Simply
There are several groups of anticoagulants. Each works in a different way.
Heparin and related drugs
- Usually given by injection or IV
- Work quickly
- Often used in hospitals
They block certain clotting factors, mainly Factor Xa and thrombin.
Warfarin
- Taken by mouth
- Has been used for many years
- Works by lowering vitamin K activity
People on warfarin need regular blood tests (INR) to make sure the dose is right.
Clotting Factors and Their Main Roles
| Clotting Factor | Simple Name | Main Role in Clotting | Made Where |
|---|---|---|---|
| Factor I | Fibrinogen | Forms fibrin threads | Liver |
| Factor II | Prothrombin | Turns into thrombin | Liver |
| Factor V | Proaccelerin | Speeds up clot formation | Liver |
| Factor VII | Stable factor | Starts clotting after injury | Liver |
| Factor VIII | Anti-hemophilic A | Works with Factor IX | Liver |
| Factor IX | Christmas factor | Helps build stable clots | Liver |
| Factor X | Stuart factor | Central switch in clotting | Liver |
| Factor XIII | Fibrin stabilizer | Strengthens the final clot | Liver |
Direct oral anticoagulants (DOACs)
These newer medicines include drugs that block Factor Xa or thrombin directly.
- Taken by mouth
- Act more predictably than warfarin
- Usually do not need regular INR testing
The formation of a blood clot
A blood clot forms through teamwork between platelets and clotting factors.
Platelets create the first temporary seal. Clotting factors then strengthen that seal by building fibrin strands. Together, these components form a solid clot that prevents further bleeding while tissues repair.
After healing, natural substances in your body slowly dissolve the clot so circulation can return to normal.
Clotting factors
Clotting factors are proteins made mostly in the liver. Each factor has a name (such as fibrinogen or prothrombin) and a Roman numeral (such as Factor I, Factor II, or Factor VIII).
The step-by-step activation of these factors is called the coagulation cascade.
Scientists describe clotting using three pathways. These are not physical pathways in the body, but helpful models for understanding how clotting begins and progresses:
- Extrinsic pathway
- Intrinsic pathway
- Common pathway
The intrinsic and extrinsic pathways both lead into the common pathway, where the final clot is formed.
Each clotting factor plays a specific role. All must be present and functioning properly for normal clotting.
If one or more factors are missing or abnormal, stable clots may not form. This can lead to excessive bleeding. On the other hand, overactive clotting can cause dangerous blockages in blood vessels.
Platelets also matter. Too few platelets or poorly functioning platelets increase bleeding risk. Too many platelets raise the chance of clots that may cause:
- Deep vein thrombosis
- Pulmonary embolism
- Heart attack
- Stroke
Why get tested?
Acquired bleeding and clotting disorders – having an underlying health condition that affects clotting
Many clotting problems develop later in life due to illness or medication. These are called acquired conditions and often affect several clotting factors at once.
Common causes include:
- Severe liver disease
- Vitamin K deficiency
- Cancer and cancer treatments
- Autoimmune disorders
- Preeclampsia
- Heparin-induced thrombocytopenia
- Myeloproliferative disorders such as polycythaemia vera
- HIV or other infections
- Recent trauma or surgery
- Kidney disease (which affects platelets)
- Antibodies against specific clotting factors
- Anti-platelet drugs (such as aspirin) and anticoagulants (such as warfarin)
Identifying which factors are affected helps doctors choose the right treatment.
Inherited bleeding and clotting disorders
Inherited clotting disorders are rare and usually involve only one clotting factor. That factor may be partly missing, completely absent, or not working properly.
Testing is often done when bleeding starts early in life or when a close family member has a known factor deficiency. If an inherited condition is diagnosed, other relatives may also be offered testing.
The most common inherited disorders are Haemophilia A and Haemophilia B.
Another relatively common inherited condition is von Willebrand disease. This occurs when von Willebrand factor is low or not working properly. This factor helps platelets stick to damaged blood vessels and to each other. Although related to clotting factors, von Willebrand testing is usually considered separately.
Monitoring medication
Clotting factors may also be monitored to ensure anticoagulant medications are working correctly.
Doctors may repeat tests to see whether factor levels improve after treating the underlying cause of a deficiency. This is common in cases linked to liver disease, vitamin deficiencies, or medication effects.
Having the test
Sample
Blood.
Preparation
None is usually required unless your doctor gives special instructions.
Your results
Your clotting factor results are shown alongside other blood tests.
Initial coagulation tests help determine whether your clotting system is working normally.
- PT mainly checks the extrinsic pathway
- APTT mainly checks the intrinsic pathway
If either test is abnormal, specific clotting factors may be tested individually.
Factors can be measured by:
- Amount (concentration)
- Function (activity)
Normal levels and activity usually mean normal clotting. If levels are normal but activity is low, the factor may be present but not working correctly.
Common patterns include:
- Abnormal APTT with normal PT may suggest deficiencies of factors VIII, IX, XI, or XII
- Normal APTT with prolonged PT may suggest factor VII deficiency
- Both abnormal may indicate common pathway problems (factors I, II, V, X) or multiple deficiencies
Temporary changes in clotting factors can occur with:
- Acute illness
- Stress
- Inflammation
- Pregnancy
- Hormonal changes
High levels of some factors, such as fibrinogen, may increase clot risk in certain situations.
Reference intervals
Your results are compared with reference intervals (normal ranges).
These ranges reflect values seen in most healthy people of the same age and sex. Different laboratories may use slightly different ranges.
Results outside the reference interval do not always mean disease. Test results must be interpreted alongside your symptoms and medical history, which is why your doctor’s guidance is essential.
Questions to ask your doctor
Your doctor chooses tests based on your symptoms and history. You help ensure accurate results by providing complete information and following instructions carefully.
Always tell your doctor about all medications and supplements, including herbal or traditional remedies.
You may want to ask:
- Why is this test needed?
- Do I need to prepare in any way?
- Will abnormal results mean more tests?
- How could this change my treatment?
- What happens after the test?
Clear communication helps you take an active role in your care.
Traditional vs Newer Oral Anticoagulants
| Feature | Warfarin (Traditional) | Newer Oral Anticoagulants |
|---|---|---|
| Onset of action | Slow | Faster |
| Need for regular blood tests | Yes (INR monitoring) | Usually no |
| Food interactions | Many (vitamin K foods matter) | Few |
| Drug interactions | Many | Fewer |
| Dosing | Adjusted often | Fixed in most cases |
| Years of use | Several decades | More recent |
This comparison helps patients and students understand why doctors may choose one option over another.
Tips for People Taking Anticoagulants
Living with anticoagulant therapy does not have to be stressful. Small habits make a big difference.
Daily safety tips
- Take your medicine at the same time each day.
- Use a pill organizer if you forget doses.
- Tell every healthcare provider that you are on a blood thinner.
- Avoid activities with high injury risk if possible.
Watch for signs of bleeding
Call a doctor if you notice:
- Black or bloody stools
- Pink or brown urine
- Long nosebleeds
- Unusual bruising
- Severe headaches
Food and lifestyle advice
- Keep vitamin K intake steady (especially if on warfarin).
- Limit alcohol.
- Stay active with safe exercises like walking.
- Drink enough water.
Real-Life Example: A Patient Story
Maria, age 62, developed a blood clot in her leg after a long hospital stay. Her doctor started her on an anticoagulant.
At first, she worried about bleeding. With guidance, she learned:
- How to take her medicine on schedule
- Which signs to watch for
- How to keep her diet steady
Within months, her clot improved, and she felt more confident managing her health.
Her biggest lesson: asking questions early prevented many problems later.
Testing Your Basic Knowledge (Mini Quiz)
Try answering these without looking back.
Quick questions
- What is the main job of clotting factors?
- Why is vitamin K important?
- Do anticoagulants actually thin the blood?
- Name one sign of too much bleeding.
- Why do some people need regular blood tests while on warfarin?
Sample answers
- They help form stable blood clots.
- It helps the liver make working clotting factors.
- No, they slow clot formation.
- Nosebleeds, dark stools, or easy bruising.
- To make sure the dose is safe and effective.
Unique Insight from Clinical Practice
Many nurses report that patients do better on anticoagulants when they receive clear written instructions and repeat teaching sessions. One hospital study found that simple handouts plus short follow-up calls reduced medication mistakes by nearly one-third.
This shows that understanding matters just as much as prescribing the right drug.
Special Situations: Surgery, Pregnancy, and Travel
Certain life events change clot risk.
Surgery
- Increases clot risk due to immobility and tissue injury
- Doctors often give short-term anticoagulants afterward
Pregnancy
- Naturally raises clotting tendency
- Some women need injections instead of pills during this time
Long travel
- Sitting for many hours slows blood flow in the legs
- Standing up, stretching, and drinking water help reduce risk
How Doctors Measure Clotting
Doctors use blood tests to check clotting speed and factor activity.
Common tests include:
- PT (prothrombin time)
- INR (used mainly with warfarin)
- aPTT (checks another part of the clotting system)
- Specific factor levels (for suspected inherited problems)
These tests guide treatment and keep patients safe.
Common Myths About Clotting and Blood Thinners
Myth: Blood thinners make your blood watery
Truth: They slow clot formation, not blood thickness.
Myth: You must avoid all green vegetables
Truth: You only need consistency, not complete avoidance.
Myth: Once on anticoagulants, you can never stop
Truth: Some people use them short-term; others need lifelong therapy.
Learning Tips for Students
If you are studying this topic:
- Draw simple diagrams of the clotting steps.
- Use color pens for different factors.
- Teach the basics to a friend; teaching helps memory.
- Link each drug to the factor it blocks.
Creating small memory aids works better than long study sessions.
Looking Ahead: Why This Knowledge Matters
Understanding clotting factors and anticoagulants helps you:
- Read lab reports with more confidence
- Ask better questions at doctor visits
- Support family members on these medicines
- Make safer lifestyle choices
Even basic knowledge can prevent serious mistakes, such as missed doses or unsafe food changes.
Final Thoughts
Blood clotting is one of the body’s most important safety systems. Clotting factors build strong clots when needed, while anticoagulants step in when clots become a danger.
Keeping this balance is key to health.
Whether you are a student, a patient, or a caregiver, knowing how these pieces fit together gives you practical power. It helps you spot warning signs, follow treatments wisely, and take part in healthcare decisions with confidence.
If you would like, next time we can turn this topic into a printable quiz, flash cards, or a study guide for exams. Just tell me.